- Anorexia Nervosa
- Arthritis
- Attention Deficit Disorder
- Autism
- Bulimia Nervosa
- Binge Eating Disorder
- Constipation
- Coronary Heart Disease
- Crohn’s Disease
- Diabetes
- Diverticular Disease
- Eating Disorders
- Food Allergies
- Food Intolerances
- Glucose intolerance
- Gout
- Hiatus Hernia
- High Blood Pressure
- High Cholesterol
- Hyperclycaemia - Increased Blood Sugar
- Hyperinsulinaemia - High Insulin Levels
- Hypoglycaemia
- Insulin Resistance
- Irritable Bowel Syndrome / Spastic Colon
- Metabolic Syndrome / Syndrome X
- Nutrient Deficiencies
- Obesity
- Poly Cystic Ovarian Syndrome
- Sports Nutrition
- Ulcerative Colitis
- Ulcers
- Weight management
• Sports nutrition
• Fertility
• Autism
• Paediatric nutrition
| ANOREXIA NERVOSA |
Anorexia Nervosa is a disorder characterized by a disturbed sense of body image, marked weight loss, morbid fear of obesity, and amenorrhea (absence of menstrual periods) in women. People suffering from this disorder think they are fat and intensely fear obesity and weight gain. They lose much more weight than is healthful. Only about 5% of cases are male. Onset is usually in adolescence, occasionally pre-pubertal, and less commonly in adulthood. Anorexia may be mild and transient, but it can also be severe and long duration. |
Dietetic approach Two phase treatment: • Short term intervention to restore body weight and save life. • Long term therapy to ameliorate long-standing problems. This will include nutritionally balanced diet plans worked out according to patient preference, evaluation of nutritional status with supplement consideration and interactive nutritional counselling on an ongoing basis. |
| ARTHRITIS |
There are around 200 kinds of arthritis, with osteoarthritis and rheumatoid arthritis being the most common. Osteoarthritis is a degenerative disease that develops as a result of wear and tear of the cartilage in a joint. Rheumatoid arthritis is an inflammatory disease in which the immune system attacks the joints. This usually lasts for years with alternating attacks and remission. |
Dietetic approach • Specific guidelines according to type and severity of arthritis. • Eliminate foods not tolerated. • Weight reduction if needed. • Identify and treat nutrient deficiencies with appropriate supplementation. |
| ATTENTION DEFICIT (HYPERACTIVITY) DISORDER (AD(H)D) |
| Definition: Developmentally inappropriate inattention and impulsivity, with or without hyperactivity. AD(H)D is implicated in learning disorders and, except for moderate to profound mental retardation, can influence the behaviour of children at any cognitive level. AD(H)D is estimated to affect 5-10% of school-aged children. |
Dietetic approach • Eliminating foods associated with hyperactivity (additives e.g. artificial colourants and flavourants) • Ensure adequate essential fatty acid intake • Blood sugar control • Eliminate Salicylates if necessary |
| AUTISM |
Autism Spectrum Disorder (ASD) is a group of diseases that is characterized by a delay in language development, impairment of social interaction, and the use of restrictive, stereotyped behaviour patterns
For most people, the breakdown of dietary protein into smaller and smaller proteins (called peptides) and finally into individual amino acids (smallest protein particle) is a process that is smoothly completed as food travels through the digestive system. However, for some autistic individuals, it has been found that a defect in the intestinal wall permits incompletely digested components (the peptides) of the original proteins to pass from the intestine into the bloodstream.
In the case of two of the diet’s most common proteins, gluten (from wheat, barley, oats, and rye) and casein (from dairy) and possible others, some of the components are released into the bloodstream where they have opioid (morphine or heroin-like) effects on the brain. Gliadorphin-7 and other similar peptides are formed in the breakdown of gluten. Bovine ß-casomorphin-7 and other similar peptides are formed in the breakdown of casein. These proteins are transported to the brain where they bind to receptors causing an effect that research indicates is manifested in some of the symptoms of autism. That is why we eliminate Gluten and Casein from the diet. Unfortunately it does not stop there; we also have to look at other biomedical dysfunctions i.e. nutrient deficiencies, leaky gut syndrome, yeast and bacteria overgrowth, impaired antioxidation and detoxification etc. |
Effects of the GFCF diet • Improved levels of attention and concentration • More calm and settled • Reduction in aggression – towards child self and others • Improved sleeping patterns • Improved communication (verbal & non-verbal) • Improved physical coordination • Improved eating habits |
Who will benefit most from the GFCF diet? Children who: • Are very young • Exhibit self-injurious behaviour e.g. head-banging, biting themselves • Exhibit overt signs of a “high” pain tolerance • Are more severely afflicted with autism – areas such as communication, social problems (eye contact, socialising), ritualistic behaviours • May have bowel problems e.g. constipation, diarrhoea, bloatedness Feeding patterns: • Diet almost exclusively gluten and/or casein • Likes strong flavours e.g. spicy food, vinegar, marmite • Habits formed on basis of “physical “ properties e.g. texture or consistency, and packaging / branding • Quantities – range from very little to excess |
My approach to implementing the GFCF diet I follow the following protocol: • Clean up the diet • BASELINE DIET • Correct vitamin and mineral deficiencies • Treat abnormal GI bugs • Probiotics / GI immune support • Digestive enzymes • Remove other offending foods • Essential fatty acids • REINTRODUCTION |
| BULIMIA NERVOSA |
| Bulimia Nervosa is characterized by recurrent episodes of binge eating during which the patient experiences a loss of control over eating and engages in either self-induced vomiting, use of laxatives and / or diuretics, or rigorous dieting, exercising or fasting to overcome the effects of the binges. Patients show a persistent over concern with body shape and weight. Patients with bulimia often are at normal weight or slightly above normal. |
Dietetic approach Two approaches: • Cognitive-behavioural. • Pharmacologic, usually administered by a psychiatrist.
The role of the dietitian is to help the patient regain control of eating habits with regular planned nutritionally balanced meals and snacks. Interactive nutritional counselling will be done on an ongoing basis. |
| BINGE EATING DISORDER |
Binge eating disorder is characterized by episodes of eating large quantities of any food in a very short period of time (without episodes of self-induced vomiting, use of laxatives and / or diuretics, fasting or excessive exercise etc. as in bulimia). Patients are usually overweight or obese and have a sense of lack of control over eating episodes. • eating more rapidly than normal • eating until uncomfortable • eating when not physically hungry • eating these foods when alone • feeling disgusted or guilty or depressed after a binge eating episode |
Dietetic approach Our first aim will be to identify trigger situations, conditional eating responses and implement solutions in accordance with a personalized eating plan. During every visit we will discuss different behavioural issues and focus on weight loss according to individual requirements. |
| CONSTIPATION |
Constipation is the difficulty or infrequent passage of faeces. Constipation can also refer to hardness of stool or a feeling of incomplete evacuation. Acute constipation represents a definite change for that individual, suggesting an organic cause, not usually treated or affected by diet. In Chronic constipation, the common functional causes are those that hamper normal bowel movements because the storage, transport, and evacuation mechanisms of the colon (large intestine) are deranged. Constipation may be a cause of poor diet, too little physical activity, too little fluid, abuse of laxatives or extra-intestinal causes. It is normal to pass a stool three times a day to once every three days. |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Assessment and correction of fibre (Non starch polysaccharides, inulins, fructo-oligosaccharides, resistant starch) fluid and probiotics intake. |
| CORONARY HEART DISEASE |
| Coronary Heart Disease (CHD) is one of the most common causes of death, particularly in the Western world. Adoption of a Western lifestyle has probably resulted in CHD now occurring more often in younger age groups, both in men and women, and is commonly a cause of premature death. CHD is a result of reduced blood flow to the heart due to a narrowing of coronary arteries called atherosclerosis. This is caused by a build up of cholesterol deposits in the walls of the arteries, or artery damage due to poor nutrition e.g. vitamin C deficiencies, inappropriate calcium supplementation, trans fatty acid intake etc. Social factors e.g. smoking also increase risk factors for CHD. |
Dietetic approach The management and prevention of CHD can require many changes inlifestyle and therefore our main aim is to implement healthy eating habits to suite your lifestyle. Topics we might look at: • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Antioxidants. • Different types of fat including, saturated, mono-unsaturated and trans fatty acids. • Lifestyle change. • Exercise. • Weight management. • Supplementation etc. |
| CROHN’S DISEASE |
| Crohn’s disease is a chronic granulamotous inflammatory bowel disease involving the small or large intestine with scarring and thickening of the bowel wall. It may be a benign course and disappear eventually, or it can become severe, with complications such as intestinal obstruction or fistula formation (an abnormal passage between two internal organs or from an internal organ to the surface of the body). When found in the small intestine, the disease is diffuse and continues to spread and damage the intestine. In Crohn’s disease, the intestinal lumen decreases, peristalsis from food intake causes cramping pain, especially in the right lower quadrant. Other symptoms include fever, weight loss, bowel narrowing, nausea, vomiting, abdominal pain and intestinal bleeding. |
Dietetic approach • Restoration of nutritional status. • With acute flare-ups an elemental (pre-digested) diet will be considered, followed by a reintroduction diet. • High energy, high protein diet with low residue intake during acute flare ups and increased fibre during remission. • Evaluation of food intolerances with an elimination diet. • Identify and treat nutrient deficiencies with appropriate supplementation. |
| DIABETES |
Diabetes is a common condition in which the amount of glucose (“sugar”) in the blood is too high. This can happen when the body does not produce enough insulin or the insulin it produces is not working effectively. Insulin is the hormone needed to convert blood glucose (“sugar”) to energy and controls blood glucose levels. There are 2 types of diabetes:
Type I Diabetes: Occurs when the pancreas stops producing insulin altogether. It usually occurs in younger people but can occur at any age. It is treated with a healthy diet and regular insulin injections.
Type II Diabetes This is the most common form of diabetes. It occurs when the body is producing some insulin but either this is not enough for its needs or the insulin is not working effectively. This type of diabetes tends to run in families. It often occurs in older people or people who are overweight. It is treated with a healthy diet although some instances this may be used in conjunction with either tablets or insulin injections.
Symptoms of uncontrolled diabetes may include: • Frequent urination • Increased thirst • Unintentional weight loss • Blurred vision • Tiredness • Dizziness • Itching • Slow wound healing |
Dietetic approach
Weight loss if needed. For type II diabetics I tend to use ketogenic weight loss programs.
Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia etc. |
| DIVERTICULAR DISEASE |
Diverticulosis is a collection of herniations of the colonic (large intestine) wall. The out-pouchings are thought to result from segmentation of the colon and the high intracolonic pressures. These may result from a diet low in fibre. In addition, the strength of the colon musculature is probably decreased. Diverticulitis develops when the accumulation of faecal matter in die diverticular pockets results in infection and inflammation, sometimes causing ulceration or even perforation. |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Initial low fibre diet with avoidance of all pips, seeds etc. This is then followed by a reintroduction of fibre and a maintenance high fibre diet. • Individual food intolerances will be assessed. |
| EATING DISORDERS |
| See Anorexia, Bulimia or Binge eating disorder. |
| FOOD ALLERGIES |
True food allergy is an immediate immune response, generally from IgE. A food allergy results from hypersensitivity to an antigen of food source (usually a protein). Allergic tendencies are mostly inherited, but not necessarily to a specific antigen. Anyone who has a tendency toward allergy may develop sensitivity to new foods. Immediate (1 minute to 2 hours) or delayed reactions (2-48 hours or longer) may occur. Symptoms may include: • Gastrointestinal • Diarrhoea
· »
Nausea
·
»
Vomiting
· »
Abdominal cramping · » Abdominal distension and pain • Skin related reaction • Respiratory reaction Most common food allergens are: milk, eggs, wheat, shellfish, tomatoes, citrus fruits, soya, and nuts. |
Dietetic approach • If allergen is known - exclude offending allergens. • If allergen is unknown do allergy tests or elimination diet to discover cause and then exclude offending allergens. • Identify and treat possible nutrient deficiencies with appropriate supplements. • Challenge patient after specific time period. |
| FOOD INTOLERANCES |
| Food intolerance is delayed food reactions, these are not antibody dependent and the reaction can be delayed for several hours or even days. This is more common than a food allergy and cannot be diagnosed through any blood or skin prick tests. Symptoms are not immediate, usually multiple and occasionally precipitate withdrawal symptoms. |
Dietetic approach • Identify intolerance through elimination diet. • Implementation of an exclusion diet. • Re-challenge after specific time period. |
| GLUCOSE INTOLERANCE |
| Glucose intolerance is when blood glucose levels are elevated, but not sufficiently high to be diagnosed as diabetes. |
Dietetic approach As for diabetes • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Weight loss if needed. I tend to use ketogenic weight loss programs.
Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia etc. |
| GOUT |
| Gout is caused by a defect in the body’s ability to metabolise uric acid. The result is an accumulation of uric acid crystals in the joints, causing pain and inflammation. Typically a single joint is involved, most commonly the base of the big toe, although the knees, wrists and ankles can also be affected. Causes of gout are uncertain, but there is often a family history. Food does not cause gout, but may trigger an attack, although it may be associated with obesity. |
Dietetic approach • Assess purine (which is converted to uric acid) intake. • Eliminate offending foods with a low purine diet plan. • Weight management if needed. |
| HIATUS HERNIA |
This is a common condition which occurs when part of the stomach forces its way into the chest through a weakness in the opening (hiatus) where the oesophagus passes through the abdominal cavity. This allows the acidic juices in the stomach to flow back into the oesophagus. The result is: • chronic heartburn • indigestion • flatulence (bloatedness) • a burning sensation in the back of the throat |
Dietetic approach • Basic guidelines to relief pain and discomfort as well as a healthy eating approach to improve overall health. • Elimination of offending foods. • Weight reduction if needed. |
| HIGH BLOOD PRESSURE / HYPERTENSION |
Hypertension is defined as systolic blood pressure ≥140 mmHg, and/or diastolic blood pressure ≥ 90 mmHg. (Normal blood pressure is 120/80) There are different types of hypertension: • Salt resistant hypertension – blood pressure that is not affected by salt intake • Salt sensitive hypertension – blood pressure that rises or falls with corresponding • Essential hypertension – hypertension of unknown etiology, also known as primary hypertension. • Secondary hypertension – hypertension secondary to another disease. |
Dietetic approach
• Nutritional assessment and healthy eating guidelines according to specific personal needs. • Identify and treat nutrient deficiencies with appropriate supplementation. • Advice according to type of hypertension. |
| HIGH CHOLESTEROL /HYPERCHOLESTEROLEMIA |
Every day the liver manufactures up to 1g of blood cholesterol, a fat-like, waxy material that is present in all cells. Blood Cholesterol is involved in the creation of certain hormones, and helps to make vitamin D and bile acids which aid digestion. Coronary heart disease is the main cause of death in South Africans following a western lifestyle. High blood cholesterol is one of the major risk factors for coronary heart disease but is one which can be controlled. It is estimated that over 4.5 million South Africans suffer from elevated cholesterol levels. Causes of high blood cholesterol levels are rooted in genetic make-up, which we can’t do anything about. But diet and obesity are also important factors which you can change.
Cholesterol can’t dissolve in the blood and therefore is carried in the bloodstream by special carriers. The two main types are LDL and HDL cholesterol.
LDL (“bad”) cholesterol: HDL (“good”) cholesterol:
Why should you care about cholesterol levels? An unhealthy diet, physical inactivity, smoking, being overweight, age and family history can lead to high cholesterol levels. High blood cholesterol levels can cause blood vessels to narrow or gradually block up. This build-up of cholesterol can happen very slowly. As the blood vessels become narrower, the flow of blood to the heart muscle is reduced. This can cause the angina (chest pain) or even a heart attack. |
Dietetic approach • Assessment of lifestyle and risk factors and nutritional intake – especially fats, sugars and alcohol. • Basic nutritional guidelines to reduce cholesterol levels. • Weight reduction if needed. • Identify and treat nutrient deficiencies with appropriate supplementation. |
| HYPERCLYCAEMIA / INCREASED BLOOD SUGAR |
Hyperglycaemia is excessive amount of glucose (“sugar”) in the blood caused by too little insulin, insulin resistance or increased food intake. Insulin is a hormone secreted by the pancreas that prevents excessive levels of glucose from accumulating in the blood, by enabling its uptake by cells.
Symptoms may include: • Frequent urination • Increased thirst • Unintentional weight loss • Blurred vision • Tiredness • Dizziness • Itching |
Dietetic approach As for diabetes • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Weight loss if needed. I tend to use ketogenic weight loss programs. Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia etc. |
| HYPERINSULINAEMIA / HIGH INSULIN LEVELS |
In Hyperinsulinism, excessive amounts of insulin are secreted in response to carbohydrate-rich foods or insulin resistance. Insulin is a hormone secreted by the pancreas that prevents excessive levels of glucose from accumulating in the blood, by enabling its uptake by cells. The result is hypoglycaemia or low blood sugar. The condition can precede diabetes or can be related to mild overt diabetes.
Symptoms include: • Light headedness • Perspiration • Sweating • Blurry vision • Increased hunger and sugar cravings |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific personal • Weight loss if needed. I tend to use ketogenic weight loss programs. Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia • Food cravings etc. |
| HYPOGLYCAEMIA / LOW BLOOD SUGAR |
Hypoglycaemia or low blood sugar is characterized by symptoms of sympathetic nervous system stimulation or dysfunction that are provoked by an abnormally low blood glucose (“sugar”) level, which has many potential causes e.g. drug induced, non-drug induced including fasting hypoglycaemia and reactive hypoglycaemia. Reactive hypoglycaemia is when your pancreas secretes too much insulin (see Hyperinsulinaemia), which lowers your blood sugar level too quickly.
In diabetes hypoglycaemia is a low blood glucose level, which can be caused by the administration of excessive insulin or oral hypoglycaemic medication, too little food, delayed or missed meals or snack, increased physical activity or alcohol intake without food. In non-diabetic persons, hypoglycaemia can occur due to poor eating habits, skipping of meals and bad food choices. Symptoms include: • Light headedness • Perspiration • Sweating • Blurry vision • Increased hunger or sugar cravings • Tiredness |
Dietetic approach • Treatment according to the cause of hypoglycaemia. • Nutritional assessment and healthy eating guidelines according to specific personal needs. • Weight loss if needed. I tend to use ketogenic weight loss programs. Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia • Food cravings etc. |
| INSULIN RESISTANCE |
| This is a condition in which the body does not respond to insulin properly, a common cause of Type II Diabetes. Thus insulin effectiveness to use glucose (“blood sugar”) is impaired. Insulin is a hormone secreted by the pancreas that prevents excessive levels of glucose from accumulating in the blood, by enabling its uptake by cells. Insulin resistance can be diagnosed when the person has a high fating Insulin level, high Triglyceride level, as well as a high waist circumference. |
Dietetic approach •
Nutritional assessment and healthy eating guidelines according to specific personal •
Weight loss if needed. I tend to use ketogenic weight loss programs.
Topics we might look at: • Glycaemic index • Food labels • Carbohydrates and sugars • Physical activity • Alcohol • Hyper and hypoglycaemia etc. |
| IRRITABLE BOWEL SYNDROME / SPASTIC COLON |
IBS (Irritable Bowel Syndrome) is the term used to describe a variety of symptoms. Symptoms vary from one individual to another and can be worse for some than others. IBS is a very common condition with around one in five people affected.
The most common symptoms are: • Diarrhoea or constipation or both • Low abdominal pain which may ease after going to the toilet • Feeling bloated • Feeling you still need to go the toilet when you have just been • Passing mucus – even on its own • A feeling of urgently needing to go to the toilet • Other symptoms may include: • Loss of appetite • Nausea or vomiting • Tiredness • Belching or excessive wind • Having to urinate urgently and feeling the need to urinate after you have just been • Pain during sexual intercourse • Worsening of symptoms during menstruation • It is not normal to pass blood! |
Dietetic approach • My aim is for the patient to be able to understand the condition. Why they get the symptoms and how to treat it. • Assessment of fibre (Non starch polysaccharides, inulins, fructo-oligosaccharides, resistant starch) intake is essential. The diet prescription is individual to the type of symptoms the patient experience. • Assessment and treatment of possible food intolerances e.g. probiotics. |
| METABOLIC SYNDROME / SYNDROME X |
Metabolic syndrome is characterized by a group of metabolic risk factors in one person. • Central obesity (excessive fat tissue in and around the abdomen) • Dyslipidaemia — primarily high triglycerides and low HDL cholesterol • Raised blood pressure (130/85 mmHg or higher) • Insulin resistance or glucose intolerance • Prothrombotic state (e.g. high fibrinogen or plasminogen activator inhibitor [–1] in the blood) • Pro-inflammatory state (e.g. elevated high-sensitivity C-reactive protein in the blood)
• overweight/obesity • physical inactivity • genetic factors
People with metabolic syndrome are at increased risk of coronary artery disease |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific risk factors. |
| NUTRIENT DEFICIENCIES |
| The most common nutrient deficiency is iron. Iron deficiency anemia (or iron deficiency anaemia) is a common anemia that occurs when iron loss (often from intestinal bleeding or menses) occurs, and/or the dietary intake or absorption of iron is insufficient. In such a state, hemoglobin, which contains iron, cannot be formed. |
Iron deficiency anemia is characterized by pallor (reduced amount of oxyhemoglobin in skin or mucous membrane), fatigue and weakness. Because it tends to develop slowly, adaptation occurs and the disease often goes unrecognized for some time. |
Other symptoms and signs of iron deficiency anemia include:
|
| Dietetic approach |
|
| POLY CYSTIC OVARIAN SYNDROME |
Polycystic Ovary Syndrome (PCOS) also known as Stein-Leventhal syndrome or functional ovarian hyperandrogenism, is a complex endocrine disorder associated with a long-term lack of ovulation (anovulation) and an excess of androgens (male hormones, e.g., testosterone).
PCOS affects 6-10% of all women and most don't even know they have it. It is treatable, but not totally curable.
Symptoms may include • Various menstrual problems • Hirsutism (excessive body or facial hair) • Endocrine abnormalities • Acne • Obesity • Infertility • Diabetes, Insulin Resistance or Hyperinsulinaemia
Even if specific symptoms are not causing an immediate problem, PCOS can have significant long-term effects, including diabetes, heart disease, and endometrial cancer.
PCOS treatment decisions depend on many factors. First line management includes diet modification, weight loss and stress reduction since obesity and stress can contribute to androgen excess. |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific personal needs with limited carbohydrate intake. • Glycaemic index and glycaemic load guidelines. • Weight reduction, usually with a ketogenic diet program. |
| SPORT NUTRITION |
| Sports nutrition is the study and practice of nutrition and diet as it relates to athletic performance. It is concerned with the type and quantity of fluid and food taken by an athlete, and deals with nutrients such as vitamins, minerals, supplements and organic substances such as carbohydrates, proteins and fats. Although an important part of many sports training regimens, it is most commonly considered in strength sports (such as weight lifting and bodybuilding) and endurance sports (for example cycling, running, triathlon). |
| Sports nutrition has many goals to enhance performance |
• First, it improves performance by improving body composition, which increases speed, quickness, mobility, and strength. • Second, it will help the speed of recovery, which will in turn create more capacity for practicing and competition as the body is becoming more fit and adjusted to the coupling of the good nutrition incorporated into the workout regimen. • Third, it will allow one to increase energy for both practice and competition, which will definitely help one's performance. • Strategic diet will also increase immunity, allowing one to stay healthy and be able to continue and intensify practice and training. Most importantly, it will improve your overall health as proper health is essential to all aspects of life. |
| ULCERATIVE COLITIS |
| Ulcerative colitis is a chronic inflammation and ulceration of the lining of the colon (large intestine) that always begins in the rectum. The intestinal musculature may also be damaged, leading to colonic dilatation (expansion of the colon, resulting in a megacolon or enlarged colon) |
Dietetic approach • Restoration of nutritional status. • With acute flare-ups use of low residue diet and in severe cases elemental (pre-digested) diet may be considered, followed by a reintroduction diet.• Increased fibre during remission. • Evaluation of food intolerances with an elimination diet. |
| ULCERS |
| A peptic ulcer is an eroded lesion in either the gastric (stomach) or duodenal (upper part of the small intestine, just below the stomach) lining. Peptic ulcers occur when the balance between the acidic digestive juices and the protective mucous membrane is disturbed. A bacterium called Helicobacter pylori may also cause peptic ulcers. |
Dietetic approach • Nutritional assessment and healthy eating guidelines according to specific symptoms. • Elimination of offending foods. |
| WEIGHT MANAGEMENT |
Obesity is a chronic, progressive, relapsing disease. Prevalence is increasing throughout the world. In many developed societies the prevalence of overweight and obesity has reached 50% of the adult population. Obesity in children is also increasing, with a doubling in obesity prevalence over the past 10-15 years (I Caterson, J Broom).
How is it assessed?
1.
Body Mass Index (BMI). This is a measure for adiposity (fatness) in adults and is valid in all but the extremes of age and in the fit and muscular. It is calculated by weight (in kg) divided by height squared (m2). |
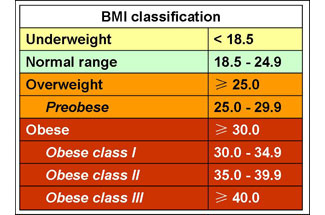 |
2. Waist circumference or waist / hip ratio. It is not just the amount of fat you have, but its site that determines the effects of being overweight. Central adiposity or fat around your middle is associated with metabolic and lifestyle diseases such as Diabetes II, Heart disease, high cholesterol, Hyperinsulinaemia, Insulin resistance etc. |
3.
Presence of risk factors or diseases. Obesity is caused by: • Genetic change - though this cause is rare. • Environmental change - we are eating inappropriately and are far more inactive. • Hormonal change - this is a rare cause of massive weight gain.
Obesity is associated with: • Metabolic disease – Type II Diabetes, Hyperinsulinaemia,Insulin Resistance, Metabolic syndrome, Dyslipidaemia (e.g. high cholesterol), Hypertension and Coronary Heart Disease. • Gastrointestinal disease – fatty liver, gallstones and steatohepatitis. • Mechanical disease – osteoarthritis, sleep problems. • Psychosocial problems |
Dietetic approach: • Nutritional assessment and healthy eating guidelines according to specific needs. • I tend to go for ketogenic weight loss programmes, depending on the individual needs, medical history and lifestyle. • Implementing of lifestyle programmes. • Assessment of possible medical imbalances. • Behaviour modification. • Every week we discuss a different topic. • Motivation!!! |